What Is Candida Albicans? Symptoms, Causes & Treatment Explained
Key takeaways
- Candida albicans normally lives on the skin, in the mouth, gut, and vagina without causing problems; it becomes an issue when it overgrows or reaches places it should not (for example, the bloodstream) (source).
- Overgrowth is more likely after antibiotics, with high-sugar diets, during hormonal shifts, or when stomach acid is suppressed by medications such as proton pump inhibitors (source, source, source).
- “Opportunistic” features—shape-shifting between forms, biofilm formation on tissues and devices, and a small toxin called candidalysin—help Candida stick, hide, and irritate tissues (source, source, source).
Candida albicans is a common yeast that most people carry without any trouble. When the balance of microbes and immune defenses changes, however, this otherwise quiet resident can overgrow and cause chronic symptoms. The overview below explains what Candida is, how overgrowth develops, the most common infections, and practical, step-by-step ways to find relief.
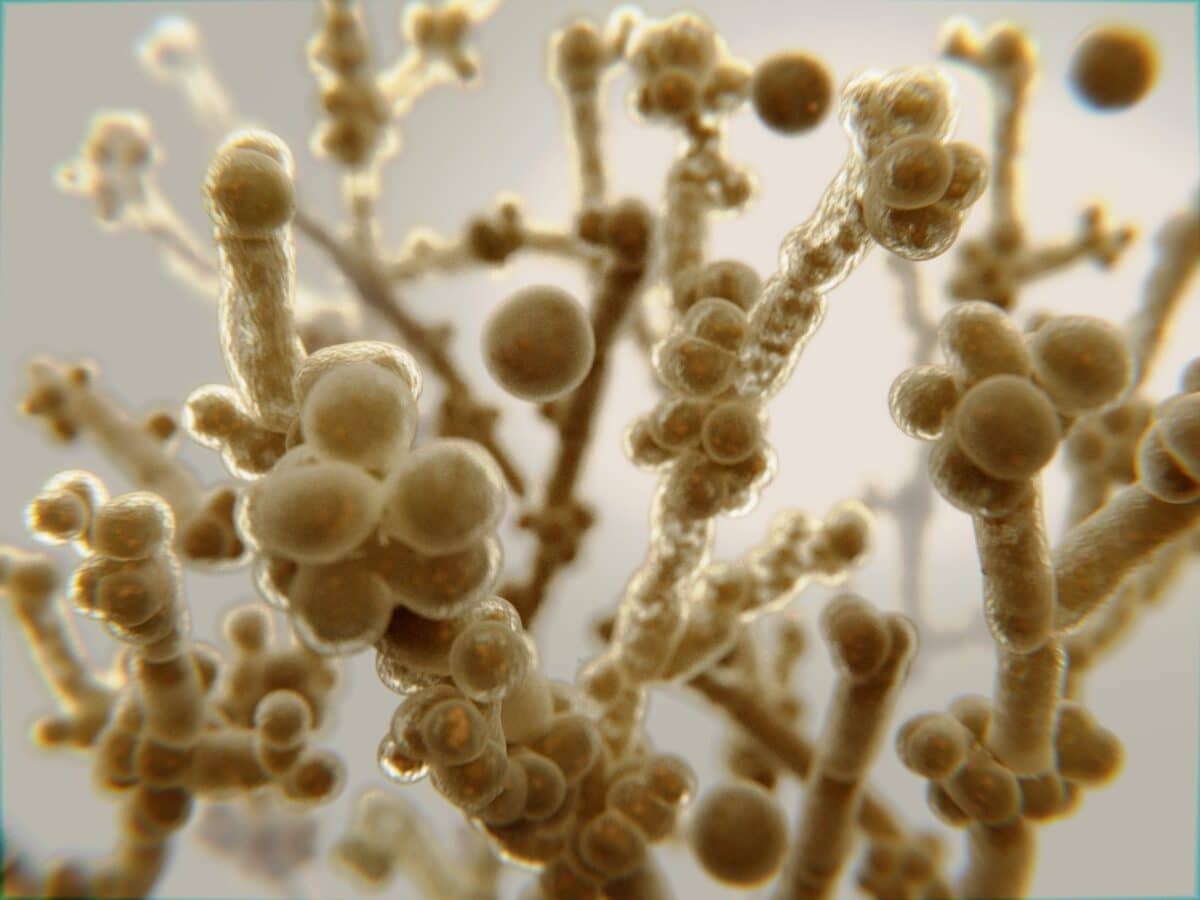
What is Candida albicans?
Candida albicans is a single-celled fungus (yeast) that lives on human skin and mucosal surfaces, including the mouth, gastrointestinal tract, and vagina. In healthy conditions, friendly bacteria and the immune system keep it in balance.
Problems arise when something tips that balance and Candida grows too much. Local infections such as oral thrush and vaginal yeast infections are common and usually manageable. Rarely, especially in people with severely weakened immunity, Candida can enter the bloodstream and cause invasive disease that requires urgent care (source, source).
To explore symptoms and next steps, see our guides to common Candida symptoms, the Candida questionnaire, and the anti-Candida diet.
Signs of overgrowth
Symptoms depend on where the overgrowth occurs. Intestinal overgrowth is often accompanied by symptoms elsewhere on the body. Always seek a clinical diagnosis because other conditions can look similar.
- Fungal skin or nail problems (for example, athlete’s foot or toenail fungus)
- Low energy or persistent fatigue; “brain fog”
- Digestive problems such as bloating, constipation, or diarrhea
- Skin complaints like eczema, psoriasis, hives, or rashes
- Vaginal itching or discharge; discomfort with intercourse
- Mouth symptoms such as white patches or soreness (oral thrush)
- Urinary irritation or rectal itching
- Seasonal allergies or strong sugar cravings
Risk increases after antibiotics; during pregnancy; with diabetes; with immune-suppressing medicines; and with long-term use of acid-suppressing drugs such as proton pump inhibitors (PPIs), which are associated with esophageal candidiasis in several studies (source, source, source, source).
Common types of Candida infection
“Candidiasis” is the umbrella term for infections caused by Candida species. Invasive candidiasis, which affects the bloodstream or organs, is uncommon in healthy people but is serious and requires urgent treatment (source).
Athlete’s foot (tinea pedis)
Typically linked to warm, moist feet and shared surfaces (locker rooms, showers). It causes peeling or itchy skin between toes and on the soles. Treat promptly and keep feet dry to prevent spread to the groin or nails.
Oral thrush
White, cottage-cheese-like patches on the tongue or inner cheeks with soreness or altered taste. It is more common in infants, denture wearers, and people who recently used antibiotics or inhaled corticosteroids. Mild cases often respond to topical antifungals; severe cases may need oral medication (source, source).
Vaginal yeast infection (vulvovaginal candidiasis)
Typical features include itching, burning, and thick discharge. C. albicans causes most cases. Many women experience at least one episode, and a subset have recurrences. Diagnosis matters because other conditions can mimic the symptoms (source, source).
Nail fungus (onychomycosis)
Nails may become thickened, discolored, and brittle; sometimes they are painful. Laboratory testing of nail debris helps target treatment.
Intestinal Candida overgrowth
This occurs when the gut microbiome becomes imbalanced and C. albicans gains an advantage. Research links high-level colonization with gastrointestinal symptoms and delayed healing in inflammatory conditions (source). Common contributors include antibiotics, high sugar intake, and chronic stress. Learn more about Candida overgrowth in the gut and the most frequent causes.
How does overgrowth develop?
Under normal circumstances, beneficial bacteria, physical barriers, and the immune system keep yeast populations in check. Overgrowth tends to happen when those defenses are weakened or the environment shifts in ways that favor Candida:
- Antibiotics and microbiome disruption. Broad-spectrum antibiotics reduce protective bacteria that usually compete with yeast, opening space for Candida to expand (source).
- Acid suppression and the upper gut. Proton pump inhibitors (PPIs) and other acid-suppressing drugs reduce stomach acidity, which can increase Candida colonization of the esophagus and stomach, and is associated with esophageal candidiasis in several settings (source, source, source, source).
- High-sugar diets. Simple carbohydrates provide quick fuel for yeast, and laboratory and animal studies show carbohydrate availability can influence Candida growth, adherence, and invasion in the gut (source, source). Reducing added sugars is a practical first step.
- Hormonal shifts. Pregnancy and higher estrogen states can alter the vaginal environment, reducing protective lactobacilli and favoring yeast overgrowth (source, source).
- Local niches and devices. Dentures, catheters, and other surfaces provide footholds for yeast to attach and form stubborn biofilms (source, source).
- Metabolic and immune factors. Diabetes and conditions that suppress immunity increase risk across many types of candidiasis (source).
The takeaway: overgrowth usually reflects a pattern—disrupted bacterial neighbors, altered pH, excess sugar, surfaces to cling to, and lowered immune surveillance. Addressing those factors is as important as treating the infection itself.
Why Candida is an opportunistic pathogen
C. albicans is well adapted to life on our mucosal surfaces. When conditions change, it can shift into “pathogen mode.” Understanding these strategies helps explain why single-step fixes rarely work.
- Shape-shifting. Candida can exist as round yeast cells or elongated filaments (hyphae). Environmental cues—including pH—help it switch forms, which changes how it moves, sticks, and invades tissues (source).
- Raising the local pH. When Candida uses amino acids as fuel, it can release ammonia that raises surrounding pH—conditions that favor the invasive hyphal form (source).
- Sticking power. Surface proteins act like “Velcro,” helping Candida grip the lining of the mouth, gut, and vagina, as well as medical materials. Two well-studied examples are Als3 and Hwp1. Als3 can also act like a doorway pass, encouraging cells to take the fungus inside—an early step in colonization and biofilm growth (source, source, source).
- Biofilms that protect and persist. Once attached, Candida builds slimy, structured biofilms that shield it from antifungals and immune cells. Biofilms form on mucosa and on devices like dentures and catheters and are a major reason some infections recur (source, source).
- A small toxin with a big impact. Hyphae produce candidalysin, a short peptide that damages epithelial membranes and triggers inflammation, contributing to soreness in mucosal infections (source, source).
- Hiding from detection. Candida can mask parts of its cell wall to blunt immune recognition, and host mucus glycans can “tame” virulence by preventing the switch to invasive forms (source, source).
How to treat Candida overgrowth
Management of the Candida overgrowth depends on the site and severity of infection. Many people do best with a combined Candida cleanse—dietary changes, probiotics, and antifungals—supported by good hygiene and attention to triggers. A simple place to start is pairing a time-release probiotic such as the Balance ONE Probiotic (third-party tested for purity and quality) with a well-designed natural antifungal blend like Balance ONE CandAssist, then layering diet and daily habits.
A low-sugar, anti-inflammatory diet
Reducing added sugars and refined carbohydrates can make the gut less hospitable to yeast. Emphasize non-starchy vegetables, quality protein, and healthy fats.
Add culinary antifungal foods—garlic, ginger, cinnamon—and consider coconut products; components such as monolaurin have shown antifungal activity in laboratory and animal studies (source, source, source).
See our lists of Candida-fighting foods and foods to avoid, and the full anti-Candida diet plan.
Probiotics
Probiotic foods (yogurt with live cultures, kefir, sauerkraut) and supplements help restore beneficial bacteria that compete with yeast.
Evidence supports a role for probiotics in reducing colonization in vulnerable groups and as adjuncts in recurrent vaginal infections, with benefits depending on strain and individual factors (source, source, source).
Our recommended option is the Balance ONE Probiotic, which is third-party tested for purity and quality and uses time-release tablets for comfortable, steady delivery.
Antifungals
For skin and vaginal infections, topical azoles are widely used; oral azoles (for example, fluconazole) may be prescribed when appropriate. For serious invasive disease, echinocandins are often first-line in clinical guidelines (source, source).
Natural antifungals—such as caprylic acid, undecylenic acid, oregano leaf extract, berberine, and garlic—can be an effective part of a gut-focused plan and are often better tolerated, with fewer systemic side effects than prescription medications for many people.
A convenient choice is Balance ONE CandAssist, a blend that combines several well-known antifungal ingredients. Start low, increase gradually, and stop if irritation occurs.
Hygiene and daily habits
- Keep skin folds and feet clean and dry; rotate shoes and wear breathable socks.
- Rinse the mouth after inhaled steroids; clean and fit dentures properly (source).
- Choose breathable underwear; change out of wet exercise gear promptly.
FAQs
Is Candida always harmful?
No. C. albicans usually lives harmlessly as part of your microbiome. It causes symptoms when it grows excessively or reaches places it does not belong (source).
How common are vaginal yeast infections?
Vaginal yeast infections are very common. Many women will experience at least one episode in their lifetime, and some have recurrent infections (source).
Can acid-reducing medicines increase risk?
Studies link proton pump inhibitors with higher colonization and a greater risk of esophageal candidiasis, likely by reducing gastric acidity and altering local defenses (source, source).
Do probiotics help?
Probiotics can reduce colonization in some settings and may help as adjuncts for recurrent vaginal infections. Benefits vary by the strains used and individual factors (source, source).
When should I see a clinician?
Seek medical advice if symptoms are severe, persistent, or recurrent; if swallowing is painful; or if you have conditions that affect immunity. Proper diagnosis ensures the right treatment (source, source).
Is an anti-Candida diet evidence-based?
Limiting added sugars and refined carbohydrates is sensible for overall health and may help create a less favorable environment for yeast. Evidence for specific named “Candida diets” is mixed, so use diet alongside other measures and personalize it to your needs (source).
Bottom line
Candida albicans is part of normal life on our skin and mucosa. Overgrowth happens when the environment shifts—after antibiotics, with high-sugar diets, during hormonal changes, or when stomach acid is suppressed.
A practical plan combines diet, probiotics, antifungals when needed, and attention to triggers. Many readers use the Balance ONE Probiotic together with Balance ONE CandAssist as part of a broader strategy—both are third-party tested for purity and quality and designed to work alongside the anti-Candida diet.

3-Month Candida Elimination Kit Start Your 3-month Candida Cleanse
This Candida Kit contains all the supplements recommended on the Candida Diet:
- LIVER ONE to process and remove the toxins created by Candida.
- CANDASSIST to inhibit and weaken the Candida colonies in your gut.
- PROBIOTIC to replace the Candida yeast with probiotic bacteria.
Plus... the CANDIDA DIET RECIPE BOOK with 50+ low-sugar recipes

Leave a Reply