Candida Auris: The Rise Of A Fungal Superbug
Just when you thought Candida albicans was bad enough, along comes a much more serious yeast overgrowth. Candida auris is an invasive form of the Candida species, and is now thought to be one of the most severe fungal infections currently in existence. In fact, it’s been referred to as a ‘fungal superbug’.
In just seven years, Candida auris has spread throughout several developed countries, which has scientists referring to it as a ‘worrisome, globally-emerging pathogen’.
The main concern with Candida auris is that it is multi-drug resistant. This means it has evolved to a point where it cannot be controlled by drugs or other anti-fungal treatments. Worse, it can spread throughout healthcare facilities such as hospitals and clinics very quickly, infecting everything in its path.
Candida albicans remains the most frequently isolated Candida species in the clinical setting. But some countries have reported a marked shift towards species of Candida with increased resistance to antifungal drugs. These include antifungals that such as fluconazole (Diflucan), the standard antifungal drug of choice in many countries, and more recently introduced antifungals known as echinocandins.
Several other species of Candida, such as Candida tropicalis, Candida glabrata, and Candida parapsilosis, are well-recognized pathogens in different geographic locations. Candida auris is a new addition to this list.
Let’s look at the details of why Candida auris is causing worldwide concern.
Table Of Contents
What is Candida Auris?
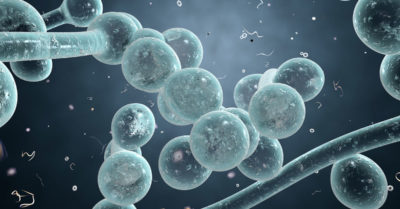
Candida auris is a deadly fungal infection causing severe disease in countries across the globe, including the US. Although related to the Candida family, it stands apart from Candida albicans for several reasons.
Candida auris is a species of ascomycetous fungus. It grows as a yeast, forming smooth, pale grey viscous colonies on its host. The first case was discovered because it appeared to continue growing even after the patient was treated with the fungicidal medication micafungin. Further examinations established the infection as a new strain of the Candida genus.
Candida auris causes invasive candidiasis (overgrowth of the candida yeast). However, unlike Candida albicans, this type of candidiasis can get into the bloodstream and become fungemia, which then spreads throughout the body, infecting the central nervous system and internal organs.
History of Candida Auris: How Did It Come About?
Candida auris was first identified in Tokyo in 2009, after it was found in the ear canal of a 70-year-old Japanese woman. In 2011, it was reported in patients in South Korea. Since then, cases have spread across Asia and Europe. The first case of Candida auris was discovered in the US in 2016.
The ease at which Candida auris spreads is be due to its ability to target patients who are already ill with another infection, or who have weakened immune systems. This is also why it tends to proliferate in hospital environments and nursing homes.
One of the reasons for the outbreak of Candida auris is increased resistance of the Candida species towards antifungal drugs. It’s believed this has happened due to widespread over-prescription of antifungal medicines.
Drugs such as fluconazole are the standard prescription antifungals used to treat fungal infections in most countries, along with newer drugs such as echinocandins. Unfortunately, when a certain medication is over-prescribed, the microbe being treated can “adapt” in a way that allows it to become resistant. These mutated strains are then referred to as ‘superbugs’ because they cannot be treated by the medication previously used.
All classes of microbes have the potential to develop resistance to a medication. For example: fungi can develop antifungal resistance; viruses can develop antiviral resistance; and bacteria can develop antibiotic resistance. Antibiotic resistance is another example of what can happen when medications are over-prescribed.
The speed at which Candida auris has spread across the world is due to its ability to be transmitted from person to person.
Why Is Candida Auris a Current Threat To People’s Health?
The ability for C. auris to wreak havoc on health environment has medical professionals around the world fearing for their patients’ lives.
Potentially Fatal
Candida auris infects the bloodstream, which can cause widespread damage to the internal organs and even death. This is particularly dangerous for those with compromised health, especially patients in hospitals or nursing homes. It’s been reported that around 30-50 percent of patients who contract Candida auris die. Of the 100+ cases of C. auris currently in the US, half are patients who were already taking antifungal medication, usually fluconazole.
Resistant To Multiple Medications
Many of the antifungal drugs used to treat infections of other Candida species are powerless against C. auris. Recent cases of C. auris have been found to be resistant to as many as three types of antifungal medicines. In fact, it can even survive harsh hospital-grade disinfectants such as chlorhexidine (Hibiclens) and bleach solutions. In some hospitals, outbreaks of C. auris have caused closures of ICUs.
On The Increase
Since its discovery in 2009, C. auris has already spread across several continents. It is currently thought to have infected people in more than a dozen countries. It has appeared mainly in healthcare facilities and clinics, and spreads through contact. This means that affected patients and contaminated surfaces or equipment pose a major risk. It’s also known that C. auris can live on surfaces for several weeks. A high standard of hygiene is crucial to preventing the spread.
Difficult To Identify
The time taken to identify C. auris plays a major part in its ability to spread. First examinations often result in the lab reporting the microbe as simply being part of a Candida species. Identification of a particular microbe as C. auris must be done in a specialized laboratory, and may take several days. During this time, the infection may be passed around the hospital environment by the unknowing patient.
In other cases, the C. auris is simply mistaken for other types of fungal infection Unfortunately, this can result in misdiagnosis and a delay in a patient receiving the necessary treatment.
What Is The Difference Between Candida Auris and Gut Imbalances Such As Candida Overgrowth?
Candida albicans is a common form of yeast that resides in the gut of most people without causing any harm. Overgrowth of Candida albicans can cause a variety of digestive problems, as well as skin conditions, hormonal disruption and vaginal thrush. Although these problems are uncomfortable and debilitating, they are not fatal.
Unlike Candida auris, Candida albicans can be treated with a variety of antifungal medications, including natural antifungals.
Also unlike Candida auris, Candida albicans cannot be transmitted from person to person. Candida auris, on the other hand, is believed to be passed between healthcare workers and their patients through contact with skin, instruments or surfaces.
Signs and Symptoms of Candida Auris
Symptoms of Candida auris infection are not always noticeable, as patients who are infected are usually already in hospital and ill with another condition, and/or already have several medical conditions.
Some typical symptoms of Candida auras infection may include:
- Fever and/or chills
- Blood poisoning (sepsis)
- Lack of response or improvement following conventional antifungal treatment
- Coma
- Organ failure
Treatment for Candida Auris: Why The Candida Diet And Natural Antifungals Aren’t Suitable
While Candida albicans may be treated through diet and natural antifungal remedies, such measures are completely ineffective with Candida auris.
The fact that Candida auris invades the bloodstream and causes organ failure means that it must be treated as soon as it is identified. It has the potential to kill a patient, and therefore only fast-acting fungal medications are suitable.
Treating Candida auris currently requires an intensive class of pharmaceutical antifungals called echinocandins. These include caspofungin (Merck’s Cancidas), anidulafungin (Pfizer’s Eraxis), or micafungin (Astellas’ Mycamine). If these powerful drugs do not work, the patient may be escalated to treatment with a highly toxic antifungal called amphotericin B.
Candia Auris vs Candia Albicans: A Matter Of Resistance
As unpleasant as Candida albicans may be, its effects and symptoms are mild compared to the harm caused by Candida auris. However, the spread of Candida auris is a reminder of how important it is to treat fungal infections with natural solutions.
The outbreak of Candida auris and its ability to resist a multitude of antifungal drugs has come about due to over-prescription of certain fungal medications. This resistance is not only less common with natural antifungal treatments, but the range of options for natural treatments is far greater. This means it’s possible to use a variety of treatments at the same time, thus reducing the chance of resistance.
If there’s one ‘good’ thing about Candida albicans, it’s that there are plenty of safe and natural antifungal remedies to fight it with! Dr Eric and I discuss these in detail in our Ultimate Candida Diet program. Be sure to check it out if you have any questions about Candida overgrowth or digestive complaints!

3-Month Candida Elimination Kit Start Your 3-month Candida Cleanse
This Candida Kit contains all the supplements recommended on the Candida Diet:
- LIVER ONE to process and remove the toxins created by Candida.
- CANDASSIST to inhibit and weaken the Candida colonies in your gut.
- PROBIOTIC to replace the Candida yeast with probiotic bacteria.
Plus... the CANDIDA DIET RECIPE BOOK with 50+ low-sugar recipes

Thank you for this information
Thank you for the continuing information from your website. I am now much better having followed your recommendations and information. I suffered from continuing overgrowth for 2 years. I have had 4 spinal surgeries since 2013 and of course antibiotics were administered during the surgeries. This past year my thyroid medication has been increased, which I feel has helped as well. I appreciate your recipes and information.
Glad to hear it, Ginny. Stay well!
I have been passing dead and alive candida for the past month. Both in stool, sweat, and my facial orifices. My body has grown considerably- though I am a 23 year-old male. The right side of my face is realigning with my left. My skin is now clearing up.
In the stool there were a few peculiar looking bugs. A few green and black. The most noteworthy one is a bulbous grey/white pearl- which I passed maybe a few times. Might this be auris? How would I go about a diagnosis?
It’s pretty safe to say that you don’t have a serious Candida auris infection. They tend to be in hospital settings and in patients whose immune systems are already compromised.
Thank You for the information I have never heard of it and it is very scary indeed..if it wasn’t for you and your help I don’t know what I would be like today .The Drs here in England have been no help to me what so ever and that upsets me.Thankyou again for all the information you send I owe you every thing.
Kindest regards Tanya
Though I’ve been suffering with candida overgrowth for 4 years, the diet, and natural anti fungals have been keeping my symptoms minimal. I was in diagnosed and untreated for an entire year which lead to my longer more difficult battle. But I strive for a natural lifestyle and I am grateful for all of the information and support. Thank you for continuing your work. And hopefully the spread of this education can help others to be informed about their condition and the risk of the western medicine approach of more and more pills. The superbug threat is growinf in so many mediums that it’s daunting and scary.
I had a candida infection since going to a ER a month ago..bad diarrhea from time to time..itchy rear..inner thighs..under arms..all come and go brain fog..come and go..fatigue come and go..low temps and mild fever and chilL come and go..itchy inner ear come and go..no one will test me for it..itchy eyes..bloating belching flatulence..headaches..joint paint in back and spine..most everything come and goes and definitely flared after I drank beer one time..